- Smoking can reduce the effects of GAHT
- Health risks increase when combined with hormones
- Trans people smoke at higher rates due to social stress, discrimination, and targeted marketing
- Nicotine replacement therapy can make quitting easier and safer (available online at Plume Clinic)
While GAHT can be a transformative and affirming process, it’s important to recognize how certain factors, such as smoking, can influence its effectiveness and overall safety. While the risks of smoking are well-known, it’s important to understand how smoking can impact those who are taking hormones as part of their transition journey. Studies have shown that transgender individuals are more likely to smoke than the general population, with rates ranging from 25% to 79%. Additionally, smoking while on GAHT can increase the risk of developing serious health issues such as blood clots, heart disease, and stroke. We believe that addressing the intersection of smoking and hormone therapy is crucial for the overall health and wellness of our community. Let’s unpack the facts and explore how medication and supportive services, such as those offered by Plume, can help you on your journey toward a smoke-free life.
Table of Contents
Understanding gender-affirming hormone therapy and smoking
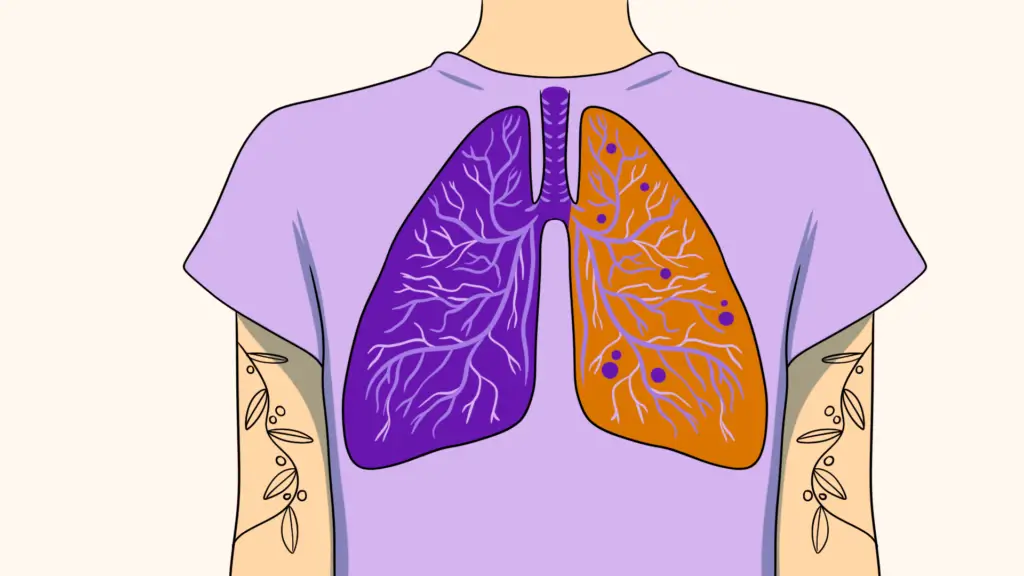
While GAHT can be a life-affirming path toward one’s true self, smoking can undermine its benefits and increase health risks. Nicotine can alter the effectiveness of the hormones involved in GAHT, potentially slowing down or reducing the expected physical changes. For example, smoking can reduce or completely cancel the efficacy of orally administered estrogens. This means that the transformative effects one hopes to achieve might not be as noticeable or could take longer to appear. Beyond the direct interaction with hormone levels, smoking carries additional risks for individuals undergoing GAHT.
The mix of smoking and hormone therapy can heighten the likelihood of encountering certain health issues. For instance, both testosterone and estrogen therapies have their set of considerations: testosterone may affect blood lipid levels, and estrogen can influence the cardiovascular system. Smoking, in combination with these hormone treatments, can amplify concerns related to heart health and blood circulation. The concern here is not just about the immediate effects, but the long-term implications that these combined risks could have on one’s health journey.
Smoking also impacts the body’s overall resilience. The immune system and the body’s ability to heal and recover can be compromised by the harmful substances in cigarettes. For someone undergoing GAHT, maintaining optimal health is crucial to support the body through the changes it’s experiencing. Smoking can counteract this, making the body more susceptible to infections and slower to heal, which could be particularly relevant during any related surgical procedures.
In recognizing these risks, the goal isn’t to overwhelm but to inform. The journey of GAHT is a deeply personal and affirming process, and understanding how smoking might affect this path allows individuals to make choices that align with their health and well-being goals. By considering the implications of smoking on GAHT, you can take proactive steps towards minimizing potential health risks, thereby supporting a smoother and more positive transition experience.
The prevalence of smoking in the transgender community
Research has consistently shown that transgender and nonbinary individuals experience higher rates of smoking compared to their cisgender counterparts in the general population. This disparity is not just a number but a reflection of the unique stressors and challenges faced by our transgender community. Factors contributing to this increased prevalence include heightened levels of social stress, discrimination, and exclusion, all of which can drive individuals towards smoking as a coping mechanism. Additionally, mental health concerns, which are more common among transgender and nonbinary people due to societal pressures and minority stress, can also play a significant role in higher smoking rates.
The targeting of marginalized communities by tobacco advertising campaigns further exacerbates this issue. These marketing strategies often prey on the vulnerabilities of our community, presenting smoking as a way to alleviate stress or fit into certain social circles. As a result, smoking becomes not only a health risk but also a social issue intertwined with the fabric of transgender and nonbinary individuals’ daily lives.
Understanding the underlying reasons behind the higher smoking rates in our transgender community is crucial for developing effective cessation programs and support systems. These programs need to be tailored specifically to address the unique challenges faced by transgender and nonbinary individuals, including combating the stigma and discrimination that contribute to the stress and mental health issues leading to higher smoking rates. Additionally, creating safe and inclusive spaces where transgender and nonbinary people can find support and resources for quitting smoking is essential.
Addressing the prevalence of smoking within our transgender community requires a multifaceted approach that considers the broader social and emotional contexts influencing tobacco use. By acknowledging and tackling these root causes, healthcare providers and support organizations can offer more meaningful and effective assistance to those looking to quit smoking, ultimately helping to close the gap in smoking rates and improve the overall well-being of transgender and nonbinary individuals.
How smoking cessation medication can help
Navigating the journey of quitting smoking can feel daunting. Fortunately, smoking cessation medication provides an effective tool to ease this path. Medications that can help you stop smoking that are safe to use while on GAHT include:
Nicotine replacement therapies (NRT). These help by supplying a controlled amount of nicotine—without the harmful chemicals found in cigarettes. This approach helps to lessen the body’s craving for nicotine and reduce withdrawal symptoms, which are often a significant hurdle in the quitting process. Over time, the dosage of nicotine is reduced, gently weaning the body off its dependency. NRT must be used cautiously in patients who have heart disease
Prescription medications take a different approach, targeting the brain’s response to nicotine. They can help to alter the way the brain reacts to nicotine, making smoking less satisfying and, thus, easier to give up. Additionally, some of these medications can help to ease the feelings of withdrawal and reduce the urge to smoke.
Bupropion (Wellbutrin) is one option. This medication can’t be used in patients who have a history of seizures, significant alcohol use, eating disorders, or who are pregnant
Varenicline (Chantix) is another option. This medication cannot be used by people who are pregnant
Incorporating these medications into a smoking cessation plan can significantly increase the likelihood of success. By diminishing the cravings and withdrawal symptoms that many fear, these medications make the goal of quitting smoking more attainable. For individuals undergoing GAHT, this means not only improving their chances of successfully quitting smoking but also optimizing the effectiveness and safety of their hormone therapy. By understanding and utilizing smoking cessation medications – such as those offered at Plume – individuals can make a significant step towards a healthier life free from smoking.